The Optic Nerve is the nerve for sight. It is like an electric cable with a million wires that carries electrical impulses from the light sensitive cells of the retina, (at the back of eye) to the brain. Our brain puts them together to form a picture. The earliest change in glaucoma is the damage to the nerve fibers which leads areas of blindness in your field of vision.
Unfortunately, people seldom notice these small blind areas until they enlarge which is why glaucoma is often called the silent thief of vision. When the entire nerve is destroyed permanent blindness results. Special tests are the only way to identify these early defects. Early detection and treatment are the keys to prevent optic nerve damage and blindness from Glaucoma (Kala Motia).
About Pressure
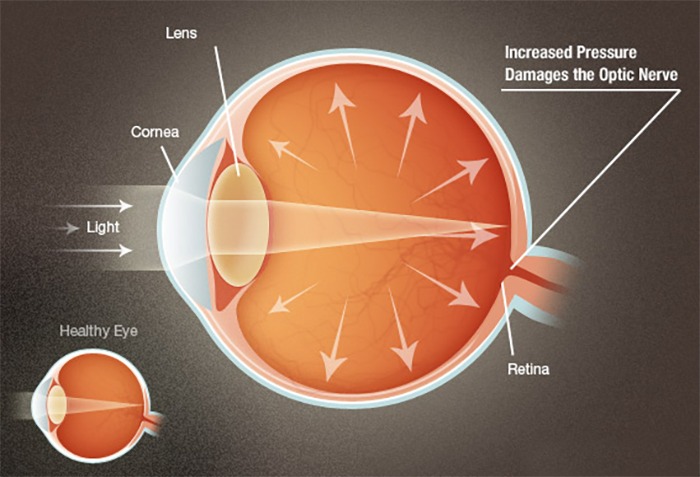
A clear fluid called the ‘Aqueous Humor’ circulates continuously within the eye. This fluid is not a part of the tears on the outer surface of the eye. Produced behind the Iris (The brown part of the eye), it flows forwards through the pupil and drains out of the eye through intricate drainage channels. Normally, fluid production and outflow are balanced. As a result the pressure inside the eye remains stable and within the safe range. If the drainage of this fluid is hampered, the pressure within the eye increases to a level that damages the cells in the optic nerve. This is Glaucoma (Kala Motia).
About Rise in pressure
The drainage portion of the eye, called the ‘drainage angle’ is like a sieve and can be blocked in different ways.
a) It may get blocked suddenly by the iris that closes the drainage angle. Eye pressure increases rapidly, resulting in a sudden loss of vision, severe eye pain and headache, rainbow halos around light accompanied by nausea and vomiting. This is called “Acute Angle Closure Glaucoma” and if not treated as an emergency it leads to permanent blindness.
b) In the second type of Glaucoma, the out flow sieves get blocked by debris. This leads to a slow rise in pressure, known as ‘Primary Open Angle Glaucoma’. Vision is lost so gradually and painlessly that a person is unaware of until the optic nerve is badly damaged. What makes it dangerous is that has no symptoms. This type of Glaucoma is much more common.
c) Glaucoma can also occur after an injury, inflammation of eye, drugs, cataract etc. Glaucoma may rarely be present at birth. The parents may notice their baby’s eye enlarging due to the increase in pressure. The cornea becomes cloudy, with watering and increasing sensitivity to light. This needs an urgent eye examination .
Range of Normal Pressure
The average Intra-Ocular Pressure (IOP; the pressure within the eye like the air pressure in tyre of a car) in adult is 16 mmHg. The actual upper limit of normal pressure, however, is difficult to pinpoint. If the 10P is consistently above 21mmHg, the chances of eye damage are probably around 10%. When the 10P is above 26mmHg, the likelihood increases to about 50%. What constitutes normal 10P is an individual matter for each person. For example, some persons with an 10P of 16mmHg may need surgery while, others with an 10P of 30mmHg may be kept under observation only. The 10P is different and independent of blood pressure. Don’t confuse it with the pressures of day to day life!
Common in all type of Glaucoma
All types of Glaucoma have three features in common. These form the basis to diagnose Glaucoma, measure the extent of damage, and monitor its progression. a) Increased 10P: The pressure inside the eye is measured with Goldmann applanation tonometer. A prism with blue lights touches the eye to accurately check 10P. There are however some types of glaucoma where damage may occur even with a normal pressure, called Normal Tension Glaucoma. b) Cupping and atrophy of the Optic Nerve: It is the drying up of the optic nerve (the nerve of sight) as it suffers damage due to high pressure inside the eye. It is assessed by examination of the fundus of the eye. c) Retinal Nevre fibre layer (RNFL) defects and Visual Field Defects: The slow death of nerve fibers is the earliest change to occur in Glaucoma. This nerve fibre layer damage is picked by a specialized instrument called OCT. Visual Fields defects are missing areas in the field of sight, though the person may be seeing well otherwise. This is measured with an instrument called a perimeter. The modern perimeter is computerized to measure; analyse, compare and report the defects.
Symptom
Unfortunately there are no symptoms in early stages. A person with Chronic Glaucoma is usually unaware of the disease. Like the hands of a clock, Chronic Glaucoma moves so slowly that its progress is not noticed. It is a silent thief of vision.
On the other hand, Acute Glaucoma, in which the pressure rises rapidly, causes severe symptoms which compel the patient to consult a doctor. Symptoms that suggest the presence of Chronic or Acute Glaucoma include are shown in above table.
Early Detection
Getting an annual eye examination at Thind Eye Hospital is the best way to detect Glaucoma. During a complete work up for Glaucoma, we will be asure your Int ra-Ocular Pres sure (Tonometry), the central corneal thickness (Pachymetry) inspect the drainage angle of the eye (Gonioscopy), evaluate for optic nerve head damage (Ophthalmoscopy), test the visual field of each eye (Perimetry) and measure the thickness of your retinal nerve fibre layer (OCT examination).
All of these tests may not be necessary for every person. But it is very important that these tests be repeated on a regular basis to monitor the progress of disease and to detect glaucoma at the earliest possible stage.
Risk Factor
People with high 10P have a higher risk of developing optic nerve damage. Other important risk factors include advancing age, severe myopia (near sighted), and a family history of Glaucoma, presence of Diabetes, past injury to the eye, surgery, or history of severe anaemia or shock.
We will weigh all these factors before deciding whether you need treatment for Glaucoma or not. If your risk of developing Glaucoma is higher than normal but there is no optic nerve damage, you will be monitored periodically as a ‘Glaucoma suspect’.
Medical Treatment
Eye drops to lower your 10P are the first line of treatment. They act to decrease eye pressure either by reducing the production of fluid within the eye or by improving the outflow through the drainage angle. It is very important to use the drops regularly at the prescribed timings.
Sometimes pills may also be required. Some medicines may occasionally result in unwanted side effects. They may sting, redden the eye and cause blurring of vision or headaches. Such side effects usually disappear after a few days. Rare side effects may be changes in your heart rate and breathing. Inform us immediately if you think you are experiencing side effects it is very important to consult your ophthalmologist before starting, stopping or changing your medication.. Frequent eye examinations and tests are the only way to monitor any changes in your Glaucoma.
Laser surgery is effective for some types of Glaucoma. In a laser surgery known as trabeculoplasty used in chronic open angle Glaucoma, the drain itself is treated In another laser surgery known as Laser iridotomy used in angle-closure Glaucoma, a hole is made in their is 0 to restore the free flow of aqueous fluid. These laser surgeries help to reduce the need for eye drops and pills to control your pressure.
In advanced cases, surgery known as trabeculectomy is necessary to control Glaucoma. We use specialized instruments to create a new drainage channel for the fluid to leave the eye, thus lowering the pressure in advanced cases. If surgery fails, special Glaucoma valves can be implanted. Fortunately, glaucoma surgery today is very safe and serious complications of modern are rare. Surgery for Glaucoma would be recommended only if the medicines or lasers fail to prevent damage to the optic nerve.
Whatever may be the approach, the objective of the treatment is to lower the eye pressure to a level at which optic nerve damage does not develop or worsen. Although eye pressure is important, the condition of your optic nerve and peripheral vision are equally or more important. It is very important to understand that achieving a normal pressure does not mean that glaucoma has been cured. It only means that the treatment is effective and would help prevent further damage to your vision. However regular eye examinations are very important while you are on treatment as glaucoma behaves differently in every patient and more aggressive treatment is often needed in some patients. This would involve reducing the pressure even further since the threshold at which pressure can cause damage is different for each individual.
The success of your treatment depends entirely on the team work put in by you and the Thind Eye Hospital team. On your part is therefore important to communicate with us and to remember to keep the follow-up appointments. If you don’t, glaucoma could be stealing your sight without your knowledge.
Management
Glaucoma is a lifelong diagnosis and treatment. Strictly speaking Glaucoma cannot be cured but it can be controlled to slow or halt optic nerve damage. The key to preventing blindness from Glaucoma is early diagnosis and treatment. This is why we emphasize regular checkups to detect glaucoma, especially if you have family history of glaucoma. If glaucoma is detected at an early stage and effective treatment is started we can prevent it from causing ANY vision loss. However achieving this goal requires a lifelong commitment to treatment and regular visits to Thind Eye Hospital.
Suggested Screening
- People with high intra-ocular pressure (IOP): Need a baseline glaucoma work up including pressure check, central corneal thickness measurement, gonioscopy, fundus examinations OCT and Perimetry. Regular follow-up visits to monitor !OP and optic nerve damage are required every six months.
- People over the age of forty years with no previous glaucoma: At least once every two years, especially whenever there is a change of reading glasses.
- Family history of Glaucoma: Regular screening form a young age for people with parents or close relatives suffering from glaucoma.
- People having high minus or plus numbered glasses: Once a year checkup.
- Other high risk factors like diabetes, eye injuries, a major eye surgery, prolonged steroid use etc., need more frequent screening


